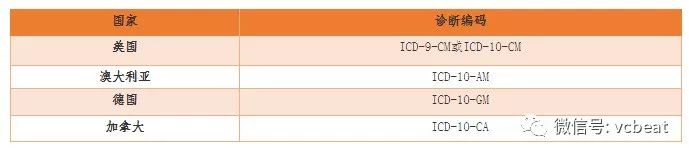
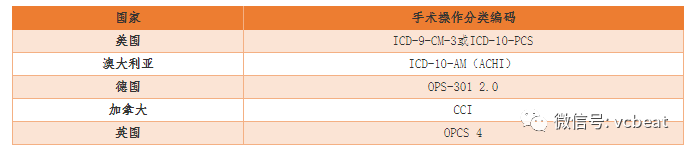
From a global perspective, the development and correct grouping of DRG systems and the determination of weights require two types of data information as the basis: one is the medical information contained in the first page of the medical record, including the diagnostic code and the operational code; the second is the cost information based on the medical record. According to the medical information, determine which DRG group each case belongs to, according to the DRG cost information, whether the homogeneity of different DRG groups is high, and if not high, whether it should be divided into different groups. Therefore, the collection and analysis of the first page data and cost data of the medical record is crucial for the correct grouping and determination of weights of the DRG. This column will introduce the international experience of collecting and analyzing the top page data and cost data of the medical record separately. (Historical Review: "One of the DRG Column Series: International Experiences in the Construction of DRG Payment System (Review)") DRG senior expert, Dr. Liu Yuchen, postdoctoral fellow in public administration at Fudan University First, what is the medical record home page The first page of the medical record is a summary of the patient's hospitalization diagnosis and treatment. It is the most concentrated, most important and core part of the information in the entire medical record. The items on the front page of the medical record basically cover all the basic information of the patient and the necessary information for DRG grouping. All information (including basic patient information, hospitalization process information, medical treatment information, cost information, etc.) is the basis for implementing DRG. The integrity and accuracy of the data on the front page of the medical record and the rigor of the quality of the original data of the medical record will directly affect the quality of the DRG group and the effect of using the grouping. Therefore, the medical staff needs to use words, symbols, codes, numbers, etc. to refine the relevant information during the hospitalization of the patient in the first page of the medical record to form a summary of the data about the patient's case. Second, the relationship between the core information of the medical record home page and the DRG group In the home page of the medical record, the name of the disease diagnosis and surgical operation should be used. This is an important basis for DRG grouping. The core idea of ​​the DRG grouping is based on commonality. The most important part of the grouping information is the diagnosis of the patient. For disease and diagnosis, the commonality is reflected in the consistency of class attribution. Therefore, the implementation of DRG must choose the appropriate disease classification method. The actual DRG grouping process needs to be processed by the computer, so the grouping process of the DRG is "coded". Different types of cases are usually distinguished by a disease diagnosis code, which is distinguished by an operation classification code, and the individual characteristics of the patient are expressed by the age, sex, birth weight (classification of the newborn case), etc. . Obviously, the diagnosis of the disease and the corresponding operation are called the key "axis" of the DRG division case. In addition, disease diagnosis and surgical operation coding are not only the basis for the development of DRG, but also the basis for determining the patient's payment for the DRG group. According to the US fiscal year 1996 medical insurance estimates, the wrong payout ratio (mainly based on disease coding errors) is 14%, totaling $23.2 billion; in 1999, the false claims rate was 8%, totaling $13.5 billion; The false claims rate was 6.8%, totaling $11.9 billion. The US Medical and Financial Administration hopes that by 2002 the false claims rate could be reduced to 5%. According to the US Office of the Superintendent, these errors are all the result of doctors providing medical information incorrectly and incorrectly coded. Therefore, standardized and unified disease diagnosis and coding can not only improve the accuracy of DRG grouping, but also ensure the effective operation of the DRG payment system, thus avoiding the unnecessary loss of medical insurance due to coding errors. Third, the development of international disease classification code As early as the 18th century, Australian basic statistician Sir George Knibbs began experimenting with the systematic classification of diseases. In 1891, the International Statistical Institute established a professional committee for the classification of causes of death, and Jacques Bertillon, head of statistical affairs in Paris, served as chairman. In 1893, Jacques Bertillon submitted a unified classification of causes of death in 1853 to the International Statistical Institute meeting in Chicago. This method was accepted and was called the Bertillon classification of causes of death. Subsequently, this method was adopted by many countries and many cities. In 1898, at the American Public Health Association meeting in Ottawa, North American countries such as the United States accepted the Bertillon classification of causes of death and recommended that they be revised once every 10 years. In 1946, WHO took over the revision of this taxonomy. Beginning with the sixth revision, this taxonomy began to be integrated into the disease classification. In 1975, the WHO released a version called the 9th revision of the International Classification of Diseases, referred to as ICD-9, which has been widely used worldwide. In 1992, WHO issued the 10th revision, named "The 10th Revision of the International Statistical Classification of Diseases and Related Health Problems", referred to as ICD-10. ICD-10 mainly refers to the etiology, location, pathology and clinical manifestations (including symptoms, signs, stages, classification, gender, age, acute and chronic onset time, etc.) when determining the classification. These properties constitute independent classification criteria. Known as the classification axis, the international disease classification ICD-10 is a multi-axis classification system. The classification distinguishes different classes by coding identifiers. The basic classes are identified by a 3-digit category code, and each category can be further divided into up to 10 Suborders, suborders are identified by the 4th digit code. The coded first bit code uses letters, the second to fourth bits each use a number, and the fourth and third bits are separated by a decimal point. For example, the code "H25.0", "H25" is a category, this category stipulates that all "early senile cataracts" are classified under this sub-head. The suborder has more details than the category, but the suborder must belong to a certain category. The classification of ICD-10 has a hierarchical refinement structure, and the coding is mutually exclusive, and a disease situation can only find an appropriate coding under one class. This and the DRG grouping need to rely on coding the hospitalization process, that is, the inconsistency of the thoughts of each hospitalized case recorded by a set of codes and indicating the information of the medical treatment. Therefore, the International Classification of Diseases (ICD) system, ICD 10, stated at the time of its publication that it was established to “allow systematic recording, analysis, interpretation and comparison of death and disease data collected in different countries or regions and at different timesâ€. “ICD is neither intended nor applicable to indexing different clinical projects. ICDs also have some control over financial research, such as billing or resource allocation.†This is a general description of the use of ICD-10 in Volume II of ICD-10. In order to meet different usage requirements, the ICD must be extended in an appropriate form, that is, code refinement. The power of code refinement comes mainly from two aspects: One is the need for clinicians to express their diagnosis based on clinical work. The International Classification of Diseases has corresponding textual descriptions of the codes used to classify them. Some of these explanatory texts are the same as the diagnostic names, some are similar to the diagnostic names, and some are quite different from the diagnostic names. A natural requirement in applying disease classification codes is to make the actual clinical diagnosis close to the disease classification in form and content. In actual work, the opposite is true. It is necessary to accept some normative or factual standard application phrases and form a diagnostic name corresponding to the code based on it. Such a result necessarily leads to the possibility that multiple diagnostic names that focus on different clinical conditions belong to one sub-head. To distinguish these diagnostic names in coding, an independent coding is required for each diagnosis, ie, a refined extension of the classification code is generated. code. Another coding refinement motivation comes from the application of classification and coding. The International Classification of Diseases has a pre-defined classification axis, a fixed axis usage order and a measure. These rules are not universally applicable, as specified by the WHO in the description of the disease classification system. Other statistical models, such as DRG, are also based on disease classification and rely on the international disease classification model, but there are differences in details. One technical means to eliminate this difference is to refine the international disease classification. This produces a refined code. In summary, regardless of the method of division, the terminology used, the degree of classification, or the ability to record, ICD-10 has a gap with clinical needs, as well as for DRG and other evaluation models. Therefore, in the implementation of DRG, countries have systematically expanded the international disease classification according to the actual clinical needs of each country, and derived the “Clinical Modification†(CM) of their own versions. The clinical version is a system developed to better characterize the patient's clinical condition. The expanded “Clinical Edition†of the International Classification of Diseases has established premise and basic requirements, including: the code cannot conflict with the standard version, and can inherit and follow the standard version of the coding principle in an appropriate manner, and can be easily and quickly converted to the standard version. Affect the use of the standard version, etc. Fourth, the development of international surgical operation classification coding ICD has been produced and developed for more than 100 years. The early international classification of diseases was not classified by surgery. However, with the understanding of medicine and the deep processing of information on hospital medical records, people realized that there is a need for a coding system. Supplement to the International Classification of Diseases. In 1959, the United States edited the classification of surgical operations as a supplement to ICD. The purpose of surgical operation classification is to standardize the different titles of the same operation and translate them into standard codes according to the principle of surgical operation classification. The classification of surgical operations is one of the main tools for processing, searching, summarizing and counting hospital medical records. . Whether in medical, research, teaching, management, or in medical payment, clinical pathways, hospital evaluation, etc., surgical operation classification has the same important role as disease classification. Later, WHO recognized the requirements for classification of medical operations in various countries. In 1978, the WHO published the International Classification of Procedures in Medicine (ICPM), including diagnosis, testing, prevention, surgery, other treatments, and Auxiliary process, etc. In the early 1980s, the WHO decided not to update the ICPM, mainly because the classification did not gain the same worldwide recognition as the ICD-9. Since in the following 20 years, there has not been a unified classification of surgical operations in various countries, some countries have developed their own standards, but they are often incompatible with each other. From the end of 2006 to the beginning of 2007, WHO decided to develop the International Classification of Health Interventions (ICHI). Most of ICHI is derived from the Australian Health Intervention Classification (ACHI), which is part of the Australian version of ICD-10.
Sample is available for Cotton Sports Towel, outdoor sports towel, soft quick dry towel, dry sports towel, waterproof dry robe, safety Reflective Safety Jacket and etc.
Welcome to discuss the details. we will give our professional suggestions and send sample for check the quality.
Certificte we have are SGS, GRS, OEKE TEX, and etc.
Cotton Sports Towel,Outdoor Sports Towel,Soft Quick Dry Towel,Dry Sports Towel Suzhou Golden Gamrnet MFG Co.,Ltd , https://www.svchangerobe.com